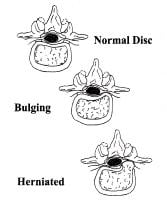
 Nuclear material is normally contained within the annulus, but it may cause bulging of the annulus or may herniate through the annulus into the spinal canal. This commonly occurs in a posterolateral location of the intervertebral disk, as depicted.
Nuclear material is normally contained within the annulus, but it may cause bulging of the annulus or may herniate through the annulus into the spinal canal. This commonly occurs in a posterolateral location of the intervertebral disk, as depicted. 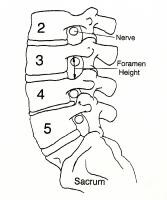 The spinal nerves exit the spinal canal through the foramina at each level. Decreased disk height causes decreased foramen height to the same degree, and the superior articular facet of the caudal vertebral body may become hypertrophic and develop a spur, which then projects toward the nerve root situated just under the pedicle. In this picture, L4-5 has loss of disk height and some facet hypertrophy, thereby encroaching on the room available for the exiting nerve root (L4). A herniated nucleus pulposus within the canal would embarrass the traversing root (L5).
The spinal nerves exit the spinal canal through the foramina at each level. Decreased disk height causes decreased foramen height to the same degree, and the superior articular facet of the caudal vertebral body may become hypertrophic and develop a spur, which then projects toward the nerve root situated just under the pedicle. In this picture, L4-5 has loss of disk height and some facet hypertrophy, thereby encroaching on the room available for the exiting nerve root (L4). A herniated nucleus pulposus within the canal would embarrass the traversing root (L5). The disc's annular structure is composed of an outer annulus fibrosus, which is a constraining ring that is composed primarily of type 1 collagen. This fibrous ring has alternating layers oriented at 60° from the horizontal to allow isovolumic rotation. That is, just as a shark swimming and turning in the water does not buckle its skin, the intervertebral disc has the ability to rotate or bend without a significant change in volume and, thus, does not affect the hydrostatic pressure of the inner portion of the disc, the nucleus pulposus.
The nucleus pulposus consists predominantly of type II collagen, proteoglycan, and hyaluronan long chains, which have regions with highly hydrophilic, branching side chains. These negatively charged regions have a strong avidity for water molecules and hydrate the nucleus or center of the disc by an osmotic swelling pressure effect. The major proteoglycan constituent is aggrecan, which is connected by link protein to the long hyaluronan. A fibril network, including a number of collagen types along with fibronectin, decorin, and lumican, contains the nucleus pulposus.
The hydraulic effect of the contained, hydrated nucleus within the annulus acts as a shock absorber to cushion the spinal column from forces that are applied to the musculoskeletal system. Each vertebra of the spinal column has an anterior centrum or body. The centra are stacked in a weightbearing column and are supported by the intervertebral discs. A corresponding posterior bony arch encloses and protects the neural elements, and each side of the posterior elements has a facet joint or articulation to allow motion.
The functional segmental unit is the combination of an anterior disc and the 2 posterior facet joints, and it provides protection for the neural elements within the acceptable constraints of clinical stability. The facet joints connect the vertebral bodies on each side of the lamina, forming the posterior arch. These joints are connected at each level by the ligamentum flavum, which is yellow because of the high elastin content and allows significant extensibility and flexibility of the spinal column.
Clinical stability has been defined as the ability of the spine under physiologic load to limit patterns of displacement so as to avoid damage or irritation to the spinal cord or nerve roots and to prevent incapacitating deformity or pain caused by structural changes.
Any disruption of the components holding the spine together (ie, ligaments, intervertebral discs, facets) decreases the clinical stability of the spine. When the spine loses enough of these components to prevent it from adequately providing the mechanical function of protection, surgery may be necessary to reestablish stability.
Recent studies
- Tomasino et al presented radiologic and clinical outcome data on patients who underwent single-level anterior cervical discectomy and fusion (ACDF) for cervical spondylosis and/or disc herniation using bioabsorbable plates for instrumentation. Overall, at 19.5 months postoperatively, 83% of the patients had favorable outcomes based on the Odom criteria. The authors found that absorbable instrumentation provides better stability than the absence of a plate but that graft subsidence and deformity rates may be higher than those associated with metal implants. In this study, the fusion rate and outcome were found to be comparable to the results achieved with metallic plates, and the authors concluded that the use of bioabsorbable plates is a reasonable alternative to metal, avoiding the need for lifelong metallic implants.
- Buchowski et al performed a cross-sectional analysis of 2 large prospective, randomized multicenter trials to evaluate the efficacy of cervical disc arthroplasty for myelopathy with a single-level abnormality localized to the disc space. The authors found that patients in both the arthroplasty and arthrodesis groups had improvement following surgery, with improvement being similar and with no worsening of myelopathy occurring in the arthroplasty group. The authors noted that although the findings at 2 years postoperatively suggest that arthroplasty is equivalent to arthrodesis in these cases, they did not evaluate the treatment of retrovertebral compression as occurs with ossification of the posterior longitudinal ligament
- Carragee et al compared progression of common degenerative findings between lumbar discs injected 10 years earlier with those same disc levels in matched subjects who were not exposed to discography. The authors found that in all graded or measured parameters, discs exposed to puncture and injection had greater progression of degenerative findings than the control (noninjected) discs. Progression of disc degeneration was 35% in the discography group, compared to 14% in the control group, with 55 new disc herniations occurring in the discography group and 22 in the control group. The study also found significantly greater loss of disc height and signal intensity in the discography discs. They noted, therefore, that careful consideration of risk and benefit are necessary in regard to disc injection.
- McGirt et al performed a prospective cohort study with standardized postoperative lumbar imaging with CT and MRI every 3 months for a year, then annually, to assess same-level recurrent disc herniation. Improvement in all outcome measures was observed 6 weeks after surgery. At 3 months after surgery, 18% loss of disc height was observed, which progressed to 26% by 2 years. In 11 (10.2%) patients, revision discectomy was required at a mean of 10.5 months after surgery. According to the authors, patients who had larger anular defects and removal of smaller disc volumes had increased risk of recurrent disc herniation, and those who had greater disc volumes removed had more progressive disc height loss by 6 months after surgery. The authors suggested, based on the findings, that in cases of larger anular defects or less aggressive disc removal, concern for recurrent herniation should be increased and that, in such cases, effective anular repair may behelpful.
- Fish et al performed a retrospective single-center study to analyze whether MRI findings can be used to predict therapeutic responses to cervical epidural steroid injections (CESI) in patients with cervical radiculopathy. Patients were categorized by the presence or absence of 4 types of cervical MRI findings: disc herniation, nerve root compromise, neuroforaminal stenosis, and central canal stenosis. The authors found that only the presence, versus the absence, of central canal stenosis was associated with significantly superior therapeutic response to CESI. They therefore concluded that the MRI finding of central canal stenosis is a potential indication that CESI may be merited.
- Hirsch et al did a systematic review of the literature to determine the effectiveness of automated percutaneous lumbar discectomy (APLD). According to the authors, based on United States Preventive Services Task Force (USPSTF) criteria, the indicated evidence for APLD is level II-2 for short- and long-term relief, indicating that APLD may provide appropriate relief in properly selected patients with contained lumbar disc prolapse. However, the authors noted that there is a paucity of randomized, controlled trials in the literature covering this subjec
{ 0 komentar... Views All / Send Comment! }
Posting Komentar